It starts with patterns. Lisa Grubb, MSN, RN director of quality management at Johns Hopkins Bayview Medical Center, conducts chart reviews with an eye for the ones that emerge around potentially preventable complications (PPCs) such as urinary tract infections from catheter use. “These don’t happen in a vacuum,” she points out. “There are always many factors surrounding them, from admissions to maintenance to patient education.”
Once she spots these trends, she begins assembling teams to study ways to reduce those complications. It’s a highly collaborative, interdisciplinary approach that has led to Johns Hopkins Bayview being named by the Maryland Health Services Cost Review Commission (HSCRC) to “the reward zone” for reducing PPCs as part of the Maryland Hospital Acquired Conditions (MHACs) initiative.
The MHACs program is a state-driven initiative first introduced in 2009 by the HSCRC and revised in 2014 that seeks to reduce hospital PPC rates by 30 percent over a five-year period. It provides financial incentives for hospitals to identify and implement measures that reduce complications.
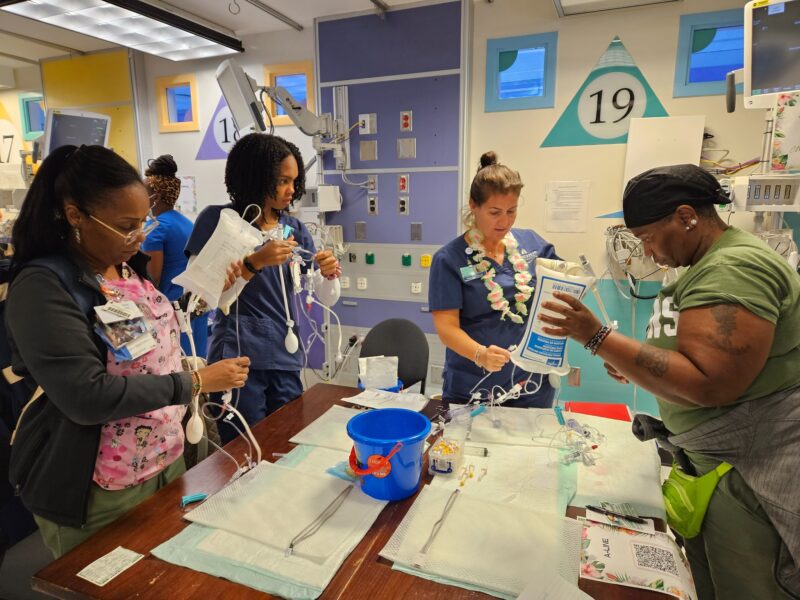
The hospital’s Quality Management Team took up the challenge soon after MHACs launched. Grubb and Janet McIntyre, MSN, RN, senior director of quality and patient safety, attended a national conference session about mechanisms of communication and problem solving for PPC reduction. They formed a multidisciplinary committee of coders, pharmacists, credentialing office attendants, and other staff as well as nurses and physicians. It meets monthly to review MHACs data to target areas of improvement. Subcommittees including a physician documentation group and action teams dig into the daily experiences of clinical staff to find the root causes of trouble spots and develop measurable solutions.
“The quality improvement teams serve as investigators trying to uncover the root causes of complications in care,” says Marcy Post, MSN, RN, clinical quality project coordinator, who leads these clinical task forces. “Often, we start out fixing one thing but it leads us to discover completely different issues.” She cites an example from the group working to address venous thrombus embolisms, where solving the problem of incomplete documentation turned up a need to expand and more carefully track equipment inventory.
Bedside nurses are crucial to successful practice changes like these because their observations serve as trail markers. Post therefore goes to great lengths to ensure that they’re heard. She expanded the size of teams from what she considers an optimal number of eight to 10 people toinclude as many as 18, knowing that only six to eight nurses will be able to leave their units to attend any given meeting. She seeks them out on the unit as well for updates and informal conversations that can yield valuable insights. “We have such committed nurses,” she says. “That’s huge. We just want to get their feedback however possible.”“I think that our nurses view the management teams as partners. We really try to understand their world, and we want them to be the ones suggesting the interventions that are then piloted in a careful, systematic way.
— Lisa Grubb, MSN, RN“I think that our nurses view the management teams as partners,” says Grubb. “We really try to understand their world, and we want them to be the ones suggesting the interventions that are then piloted in a careful, systematic way.”
That spirit of collaboration and exchange extends beyond MHACs team meetings, as the participants welcome opportunities to share their success strategies with many different audiences. The physician documentation committee has produced physician champions who now serve on a state task force to help establish a standard statewide definition for four areas of difficulty. Grubb routinely presents to a variety of groups including faculty and trustees, and she and Post validate outcomes through discussions at professional practice council meetings. “We want to see what makes a significant difference for the MHACs program, but also for the staff and patients,” emphasizes Grubb. “We’re taking a holistic approach to improve practice and make an easier path for everyone. No matter what, we’re going to impact the patient when each of us succeeds.”
Photo by Chris Hartlove